Atopic Dermatitis Articles
Safety andTolerance Evaluation of a Suncare Product in Ethnically Diverse Children With Atopic Dermatitis-Prone Skin
Atopic Dermatitis (AD) is a common chronic inflammatory skin condition, with high prevalence in children. Sun protection is important for children with eczema and AD-prone skin, yet many sunscreens can cause skin irritation due to their formulations. In this study, we evaluated the safety and tolerance of an SPF 50 sunscreen in ethnically diverse children with a history of AD over 4 weeks of product use
Mycosis Fungoides Palmaris et Plantaris Mimicking Dyshidrotic Eczema: A Case Report
This case report presents a middle-aged woman with MFPP whose initial presentation was mistaken for dyshidrotic eczema. Despite treatment with topical corticosteroids, the patient’s lesions persisted, prompting further investigations that led to the diagnosis of MFPP.
Image Analysis of Xerosis and Atopic Dermatitis Following Prebiotic Skincare Regimen in Ethnically Diverse Patients
Variations in the epidemiology, clinical presentation, and disease course in atopic dermatitis (AD) patients with Skin of Color (SOC) compared with white counterparts have been reported. In this study, we evaluated the capability of a new imaging device (SkinCam) in quantifying skin texture changes in diverse patients, presenting with AD or xerosis, after using a prebiotic skincare routine over 10 weeks.
Ant Venom-Based Ceramide Therapy Is Effective Against Atopic Dermatitis In Vivo
Background: Atopic dermatitis (AD) is a common skin condition with relatively few therapeutic alternatives. These include corticosteroids, which address inflammation but not superinfection, and Januse…
Selection of Nemolizumab Clinical Dosage for Atopic Dermatitis
Nemolizumab is a monoclonal antibody directed against the interleukin-31 receptor A subunit, which is involved in the pathogenesis of pruritus and inflammation in atopic dermatitis (AD). Clinical tria…
Cross-Sectional Study of Psoriasis, Atopic Dermatitis, Rosacea, and Alopecia Areata Suggests Association With Cardiovascular Diseases
Background: A growing body of evidence suggests that several inflammatory skin diseases (ISDs) are associated with systemic inflammation and cardiovascular disease (CVDs). Methods: We used the TriNet…
Sequential Treatment With Topical Trifarotene and Injectable NASHA Gel in Acne Scars: A Case Series
Background: Topical retinoids are a mainstay in acne management and have been shown to improve skin texture. Injectable non-animal stabilized hyaluronic acid (NASHATM) gel as skin booster is largely used in aesthetic treatments to improve skin quality including the appearance of atrophic acne scars.
A Qualitative Study on Product’s Impact on Atopic Dermatitis Among Adolescent and Adult Patients
Objective: To qualitatively assess the life experiences and impact of treatment in adult and adolescent patients with AD being treated with this product.
The Safety and Efficacy of Roflumilast Cream 0.15% and 0.05% in Patients With Atopic Dermatitis: Randomized, Double-Blind, Phase 2 Proof of Concept Study
Background: Patients with atopic dermatitis (AD) need safe and effective topical treatments.
Objective: To assess safety and efficacy of a specific cream in patients with mild to moderate AD.
Analysis of Reddit Reveals Dupilumab Questions Among Atopic Dermatitis Patients
Atopic dermatitis patients are turning to social media to seek guidance and source medical information. Reddit, the seventh most visited website in the US, contains the popular “eczeMABs” subreddit, a forum dedicated to discussing monoclonal antibody therapy for atopic dermatitis.
Patient Questions about Atopic Dermatitis from Reddit
Atopic dermatitis and eczema patient questions remain unanswered as they turn to Reddit. Reddit, the seventh most visited website in the US with approximately 430 million monthly active users, has become a popular platform for patients to source medical information and discuss diseases. See their questions, frustrations and insights.
The Heterogeneity of Atopic Dermatitis
Atopic dermatitis (AD) is a chronic and burdensome inflammatory skin disease. This narrow and overly simplified description overlooks the heterogeneity of AD. While itch is the most prevalent and burdensome symptom of AD,skin-pain is one of several other symptoms that contribute to disease-burden.
Development and Evaluation of an Atopic Dermatitis Care Plan for Providers
Collette Utley DNP FNP-BC PNP-BC, Michael H. Gold MD FAAD, Melissa Hall DNP FNP-BC AGPNP-BC J Drugs Dermatol. 2020;19(10): 950-955. doi:10.36849/JDD.2020.5090
A universal AD care plan was developed to improve AD disease management and patient outcomes. Post-implementation of providers’ perceptions was assessed for how the AD universal care plan affected their ability to provide patient education.
Topical Agents Currently in Phase II or Phase III Trials for Atopic Dermatitis
Shelley K. Uppal BS, Vipawee S. Chat BA, Donovan G. Kearns BS, Jashin J. Wu MD J Drugs Dermatol. 2020;19(10):956-959. doi:10.36849/JDD.2020.5214
A systemic literature review was performed to examine the safety and efficacy of topical agents currently in phase II and phase III clinical trials for AD. Our team searched the databases, PubMed, Google Scholar, and ClinicalTrials.gov, on March 2020 for studies pertaining to the use of topical agents in AD. Key words included each drug or “topical agents” combined with “atopic dermatitis.”
The ABC Topical Management of Atopic Dermatitis in Philippines: Expert Recommendations
Angela M Lavadia MD, Angela T Cumagun MD, Lourdes Palmero MD, Noemie Salta Ramos MD, Cindy Jao Tan MD J Drugs Dermatol. 2021;20(1):84-87. doi:10.36849/JDD.2021.5080
An ABC scheme of atopic dermatitis (AD) management entails anti-inflammatory, barrier repair and basic skin care strategies to adequately manage AD. It is an easy-to-follow model which helps lessen distress and improve the quality of life amongst patients. This scientific expert panel, likewise, seeks to provide guidance for all healthcare professionals involved in the care and management of AD patients.
Atopic Dermatitis and the Role of the Skin Microbiome in Choosing Prevention, Treatment, and Maintenance Options
Hilary Baldwin MD, Crystal Aguh MD, Anneke Andriessen PhD, Latanya Benjamin MD FAAP FAAD, Aaron S. Ferberg MD, Deirdre Hooper MD FAAD, Joseph L. Jarizzo MD, Peter A. Lio MD, Brook Tlougan MD FAADI, Heather C. Woolery-Lloyd MD, Joshua Zeichner MD FAAD J Drugs Dermatol. 2020;19(10):935-940. doi:10.36849/JDD.2020.5393
Atopic dermatitis (AD) is a common skin condition characterized by disturbed barrier function, skin inflammation, and cutaneous dysbiosis. Clinically, it manifests as chronic-recurrent xerosis, pruritus, and erythematous lesions. Its pathophysiology is complex, making the selection of appropriate treatment options a task.
Atopic Dermatitis: A Review of Current Diagnostic Criteria and a Proposed Update to Management
Matthew Reynolds PA-C, Joe Gorelick RN MSN FNP-C, Matthew Bruno PA-C J Drugs Dermatol. 2020;19(3): doi:10.36849/JDD.2020.4737
The objective of this review is to describe the current thinking on the clinical features of AD alongside current treatment guidelines, in order to consolidate and distill past and current criteria used in AD diagnosis, and thereby propose a more simplified set of diagnostic criteria.
Topical Agents for the Treatment of Atopic Dermatitis
Lawrence F. Eichenfield MD, Thomas Luger MD, Kim Papp MD, et al. J Drugs Dermatol. 2020;19(1):50-64. doi:10.36849/JDD.2020.4508
This review summarizes the efficacy and safety data of topical therapies including corticosteroids, calcineurin inhibitors, and crisaborole and it shows that comparison among available agents is difficult because of conflicting methodologies used across clinical trials and that there is considerable variability in safety reporting among AD trials.
A Global Review on the Risk Factors and Management of Early Atopic Dermatitis in Children Ages 0 to 2 Years Old
Lawrence A. Schachner MD FAAD FAAP, Adelaide A. Hebert MD FAAD, Anneke Andriessen PhD, Latanya T. Benjamin MD FAAD FAAP, et al. J Drugs Dermatol. 2019;18(10):1020-1027.
The current review aims to explore early intervention in infants and young children with eczema and AD-prone skin by improving skin barrier function and controlling inflammation at the earliest time point using a moisturizer and a proactive treatment.
Dupilumab in Dermatology: Potential for Uses Beyond Atopic Dermatitis
Nolan J. Maloney BS,Kyle Tegtmeyer BS, Jeffrey Zhao BA, Scott Worswick MD J Drugs Dermatol. 2019;18(10):1053-1055.
Given that dupilumab is relatively well tolerated and has shown efficacy in diseases mediated by Th2 processes, a new topic of interest is whether dupilumab might prove effective in other conditions in dermatology.
Prescribing Patterns for Atopic Dermatitis in the United States
Adrian Pona MD, Abigail Cline MD PhD, Sree S. Kolli BA, Steven R. Feldman MD PhD, Alan B. Fleischer Jr. MD J Drugs Dermatol. 2019;18(10):987-990.
Although pediatricians manage more AD visits than dermatologists in total visits, dermatologists manage more AD visits than pediatricians per physician. Characterizing how AD patients are currently treated may build a reference for future clinical research investigating novel standard-of-care treatment in AD.
Efficacy of Dupilumab in Different Racial Subgroups of Adults With Moderate-to-Severe Atopic Dermatitis in Three Randomized, Placebo-Controlled Phase 3 Trials
Andrew F. Alexis MD MPH, Marta Rendon MD, Jonathan I. Silverberg MD, David M. Pariser MD, et al. J Drugs Dermatol. 2019;18(8):804-813. ClinicalTrials.gov identifiers: NCT02277743, NCT02277769, NCT02260986
Significant clinical improvement and a favorable benefit-risk profile can be achieved with dupilumab treatment in patients of White, Asian, and Black/African American racial subgroups with moderate-to-severe AD inadequately controlled with topical medications.
Systemic Therapies for Moderate-to-Severe Atopic Dermatitis: Expert Perspectives in Practice
Mark Lebwohl MD, Andrew F. Alexis MD MPH, Lisa A. Beck MD, et al. J Drugs Dermatol. 2019;18(2):122-129.
Recently published expert perspectives outlined recommendations for the diagnosis and treatment of moderate-to-severe AD in adults, reflecting evidence-based, practical recommendations to support allergists and dermatologists in selecting appropriate treatment in the era of biologic therapies. In these case studies, we demonstrate how AD severity, treatment response, and treatment failure can be assessed, and the role of emerging systemic treatments in the management of moderate-to-severe AD.
Economic Evaluation of Dupilumab for Moderate-to-Severe Atopic Dermatitis: A Cost-Utility Analysis
Marita Zimmermann MPH PhD, David Rind MD MSc, Rick Chapman PhD, MS, et al. J Drugs Dermatol. 2018;17(7):750-756.
Moderate-to-severe atopic dermatitis can be difficult and costly to treat. We aimed to identify the cost-effectiveness of dupilumab compared to usual care in moderate-to-severe atopic dermatitis.
Trends in Atopic Dermatitis Management: Comparison of 1990-1997 to 2003-2012
Alice He BS, Steven R. Feldman MD PhD, and Alan B. Fleischer Jr. MD J Drugs Dermatol. 2018;17(2):135-140.
Atopic dermatitis (AD) is primarily treated with topical therapies, systemic immunosuppressants, or adjunctive therapies. As novel treatment approaches for AD emerge, we characterize AD treatment and examine trends in treatment over time.
Sponsored
Podcast Episodes
Choosing Wisely: Capitalizing on Atopic Dermatitis Clinical Trial Data for Meaningful Selection of Topical Agents
We are finally getting what we asked for: Pharma is ponying up for head to head studies to provide us with meaningful data to help make better clinical decisions. However, these valuable projects are often with systemic agents, such as biologics, leaving topical treatments in the dust. To address this, Dr. Lawrence Eichenfield, Professor of Dermatology and Pediatrics, UCSD, and colleagues sought to make the most out of the data we do have on the litany of topical options for atopic dermatitis and provide efficacy and safety guidance (A for effort!). Tune in to hear what this dream team concocted about creams. Hear how an expert approaches new atopic dermatitis patients. Don’t miss out – this is all very topical.
Trending Now: Shifts and Gaps in Atopic Dermatitis Management by Derm and Non-Derm Physicians
Back by popular demand, Dr. Steven Feldman, Professor of Dermatology, Pathology and Public Health joins host Dr. Adam Friedman from GW School of Medicine to review his recent database dive entitled “Trends in Atopic Dermatitis Management: Comparison of 1990-1997 to 2003-2012.” What new trends, both good and bad, have emerged? What can we expect and hope for the future of AD care? What tricks of the trade do these two employ when utilizing systemic immunosuppressants? Itching for answers? Make sure to tune in…
Go superpotent or go home: The utility and safety of Class 1 topical steroids
In this edition of the JDD Podcast, Ask the Investigator, host Dr. Adam Friedman digs deep with UCSF Assistant Professor of Dermatology Dr. Tina Bhutani to powerlift the most up to date safety data on Class 1 superpotent topical steroids from her study entitled “Update on the Systemic Risks of Superpotent Topical Steroids.” Is steroid phobia valid, or does proper use of steroids properly protect from the adverse event boogeyman. Hear from the expert how to effectively use topical steroids while limiting local and systemic side effects, and how to get your patients on board, especially those nay sayers. Do not miss this clinically relevant and im-POTENT podcast ( nailed it!).
We’re Not Alone: The role of the cutaneous microbiota in maintaining skin health
In this special edition of the JDD podcast, with consideration from La Roche-Posay, host Dr. Adam Friedman is joined by Acne guru Dr. Hilary Baldwin, Director of the Acne Research Center and Associate Professor of Dermatology at SUNY Downstate, to review the cutting edge of cutaneous microbiome research and translational applications. Yes you are covered in bacteria – accept it, own it, and love it. Learn how harmony between the >500 species on our skin keep our barrier and cutaneous immunity in check, and conversely, how dysbiosis can facilitate a broad range of cutaneous pathology. This special edition is not to be missed!
Translational Lecture Series
Targeting cAMP Signaling for the Treatment of Inflammatory Diseases of the Skin
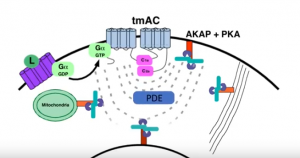 Dr. Jon Zippin, Assistant Attending Dermatologist and Assistant Professor of Dermatology at Weill Medical College of Cornell, elucidates the complexity of cAMP biology and the translational impact of PDE4 inhibition as it relates to chronic inflammatory skin diseases. Tune in to learn why targeting this pathway is clinically meaningful but also where more work is needed to improve outcomes.
Dr. Jon Zippin, Assistant Attending Dermatologist and Assistant Professor of Dermatology at Weill Medical College of Cornell, elucidates the complexity of cAMP biology and the translational impact of PDE4 inhibition as it relates to chronic inflammatory skin diseases. Tune in to learn why targeting this pathway is clinically meaningful but also where more work is needed to improve outcomes.
Update on Pediatric Inflammatory Skin Disorders: How Pathogenesis Informs Treatment
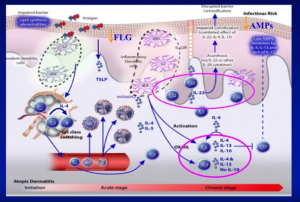 Dr. Amy Paller, Walter J. Hamlin Professor and Chair of Dermatology & Professor of Pediatrics at Northwestern University Feinberg School of Medicine in Chicago, Illinois, delivers a presentation discussing the cause and treatment of pediatric Atopic Dematitis, including co-morbidities, epidermal barrier impairment, and compliance issues.
Dr. Amy Paller, Walter J. Hamlin Professor and Chair of Dermatology & Professor of Pediatrics at Northwestern University Feinberg School of Medicine in Chicago, Illinois, delivers a presentation discussing the cause and treatment of pediatric Atopic Dematitis, including co-morbidities, epidermal barrier impairment, and compliance issues.
Itch form Bedside to Bench
 Dr. Gil Yosipovitch, Professor of Dermatology at University of Miami Miller School of Medicine, provides residents and physicians access to the latest bench research and practical pearls from a master in pruritus that will help them offer the highest quality evidence-based dermatological care.
Dr. Gil Yosipovitch, Professor of Dermatology at University of Miami Miller School of Medicine, provides residents and physicians access to the latest bench research and practical pearls from a master in pruritus that will help them offer the highest quality evidence-based dermatological care.
JDD Blog

Guselkumab Efficacy by Psoriasis Disease Severity and Treatment History: VOYAGE 1 and 2 Post Hoc Analyses









