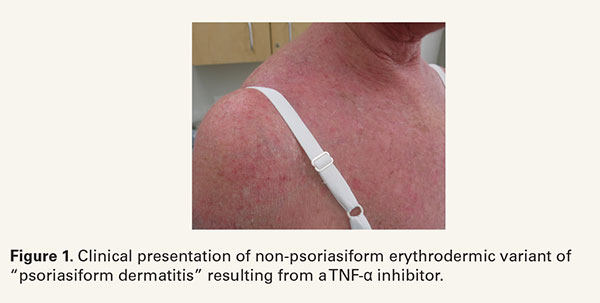
Tumor necrosis factor-α inhibitors (TNFIs) have significantly improved the quality of life for patients with psoriasis and psoriatic arthritis. Despite their beneficial effects, TNFIs have been reported to cause paradoxical ‘psoriasiform’ eruptions.1 Although this nomenclature has become pervasive in the dermatology lexicon, there is a growing body of literature highlighting the protean clinical presentation of this eruption (Figure 1), which could ultimately lead to a delayed diagnosis.2-5 The diversity of the morphology highlights the importance of identifying key histopathologic characteristics, which to date have not been well-characterized.2
In the current literature, interface dermatitis can be prevalent histologically amongst TNFI-induced ‘psoriasiform’ lesion biopsies.3-5 In a case series by Laga and colleagues, four among 16 biopsies for morphologically psoriasiform lesions showed interface/lichenoid dermatitis.3 Instead of typical psoriasiform hyperplasia with hypogranulosis, confluent parakeratosis, and lymphocytic infiltrate, these biopsies showed epidermal hyperplasia with hypergranulosis, eosinophilic cytoid bodies, orthokeratosis, and band-like lymphocytic infiltrate at the dermoepidermal junction. Additional case series have also reported focal interface/lichenoid dermatitis with predominant CD8+ T-cell infiltrate in the upper dermis.4,5 Similarly, vacuolar interface dermatitis can be present in TNFIinduced ‘psoriasiform’ eruptions with vacuolization at the dermoepidermal junction (Figure 2).
Importantly, while spongiosis is not a common pathologic feature for psoriasis (more often dependent on biopsy site selection), spongiotic dermatitis is known to be prevalent amongst TNFI-induced ‘psoriasiform’ eruptions.2,4,5 Hu and colleagues found that 35% of TNFI-induced ‘psoriasiform’ biopsies demonstrated spongiotic dermatitis.2 Similarly, eosinophil-rich perivascular pattern dermatitis may be seen in TNFI-induced ‘psoriasiform’ eruptions.3,5,6
Few studies also observed histopathologic findings of folliculitis on TNFI-induced ‘psoriasiform’ lesion biopsies.2,3 Given that some TNFI-induced psoriasiform eruptions may involve the hair follicle, it becomes important to further biopsy areas that do involve hair follicles to verify true psoriasiform dermatitis over folliculitis.
The correlation with histopathologic characteristics and morphology of TNFI-induced eruptions is crucial for diagnosis and differentiation from other cutaneous adverse events of TNFI therapy.6 However, the broad use of the terms TNFI-induced ‘psoriasis’ or ‘psoriasiform lesions’ creates an inconsistency between clinical morphology and histologic findings, which can obscure the true diagnosis and delay proper treatment. For example, some TNFI-induced ‘psoriasiform’ eruptions will improve with withdrawal of TNFI while other eruptions will worsen even though they fall under the same TNFI-induced ‘psoriasiform’ category.2,4,7 Based on the mounting evidence in the literature that TNFI-induced ‘psoriasiform’ eruptions present with a wide spectrum of overlapping morphology and histopathologic features, the characterization of TNFI-induced lesions should rely more on the histopathologic pattern.6,7 Therefore, it is certainly warranted to histologically evaluate new cutaneous eruptions of patients on TNFI-based therapy, and the nomenclature should be changed to reflect the unique attributes of this condition.
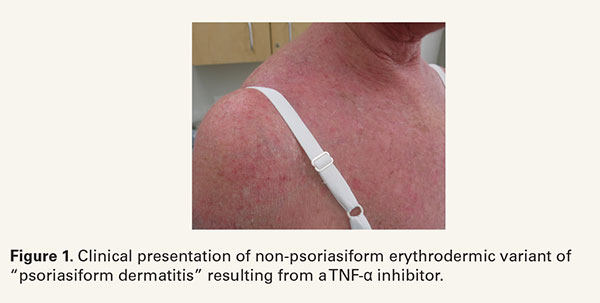

In the current literature, interface dermatitis can be prevalent histologically amongst TNFI-induced ‘psoriasiform’ lesion biopsies.3-5 In a case series by Laga and colleagues, four among 16 biopsies for morphologically psoriasiform lesions showed interface/lichenoid dermatitis.3 Instead of typical psoriasiform hyperplasia with hypogranulosis, confluent parakeratosis, and lymphocytic infiltrate, these biopsies showed epidermal hyperplasia with hypergranulosis, eosinophilic cytoid bodies, orthokeratosis, and band-like lymphocytic infiltrate at the dermoepidermal junction. Additional case series have also reported focal interface/lichenoid dermatitis with predominant CD8+ T-cell infiltrate in the upper dermis.4,5 Similarly, vacuolar interface dermatitis can be present in TNFIinduced ‘psoriasiform’ eruptions with vacuolization at the dermoepidermal junction (Figure 2).
Importantly, while spongiosis is not a common pathologic feature for psoriasis (more often dependent on biopsy site selection), spongiotic dermatitis is known to be prevalent amongst TNFI-induced ‘psoriasiform’ eruptions.2,4,5 Hu and colleagues found that 35% of TNFI-induced ‘psoriasiform’ biopsies demonstrated spongiotic dermatitis.2 Similarly, eosinophil-rich perivascular pattern dermatitis may be seen in TNFI-induced ‘psoriasiform’ eruptions.3,5,6
Few studies also observed histopathologic findings of folliculitis on TNFI-induced ‘psoriasiform’ lesion biopsies.2,3 Given that some TNFI-induced psoriasiform eruptions may involve the hair follicle, it becomes important to further biopsy areas that do involve hair follicles to verify true psoriasiform dermatitis over folliculitis.
The correlation with histopathologic characteristics and morphology of TNFI-induced eruptions is crucial for diagnosis and differentiation from other cutaneous adverse events of TNFI therapy.6 However, the broad use of the terms TNFI-induced ‘psoriasis’ or ‘psoriasiform lesions’ creates an inconsistency between clinical morphology and histologic findings, which can obscure the true diagnosis and delay proper treatment. For example, some TNFI-induced ‘psoriasiform’ eruptions will improve with withdrawal of TNFI while other eruptions will worsen even though they fall under the same TNFI-induced ‘psoriasiform’ category.2,4,7 Based on the mounting evidence in the literature that TNFI-induced ‘psoriasiform’ eruptions present with a wide spectrum of overlapping morphology and histopathologic features, the characterization of TNFI-induced lesions should rely more on the histopathologic pattern.6,7 Therefore, it is certainly warranted to histologically evaluate new cutaneous eruptions of patients on TNFI-based therapy, and the nomenclature should be changed to reflect the unique attributes of this condition.